 Lab Vision:
Lab Vision:
We envision a future where precision immunomodulation prevents respiratory infections before they begin. Our lab seeks to lead this transformation by uncovering how chronic lung disease modifies host-pathogen interactions and leveraging that knowledge to design durable, cross-cutting therapies.
Lab Mission:
To investigate how allergic immune systems respond to non-allergic insults, while fostering a collaborative and inclusive lab culture committed to curiosity, rigor, and translational impact.
 Investigating antiviral immune responses in allergic asthma during common respiratory viral infections
Investigating antiviral immune responses in allergic asthma during common respiratory viral infections
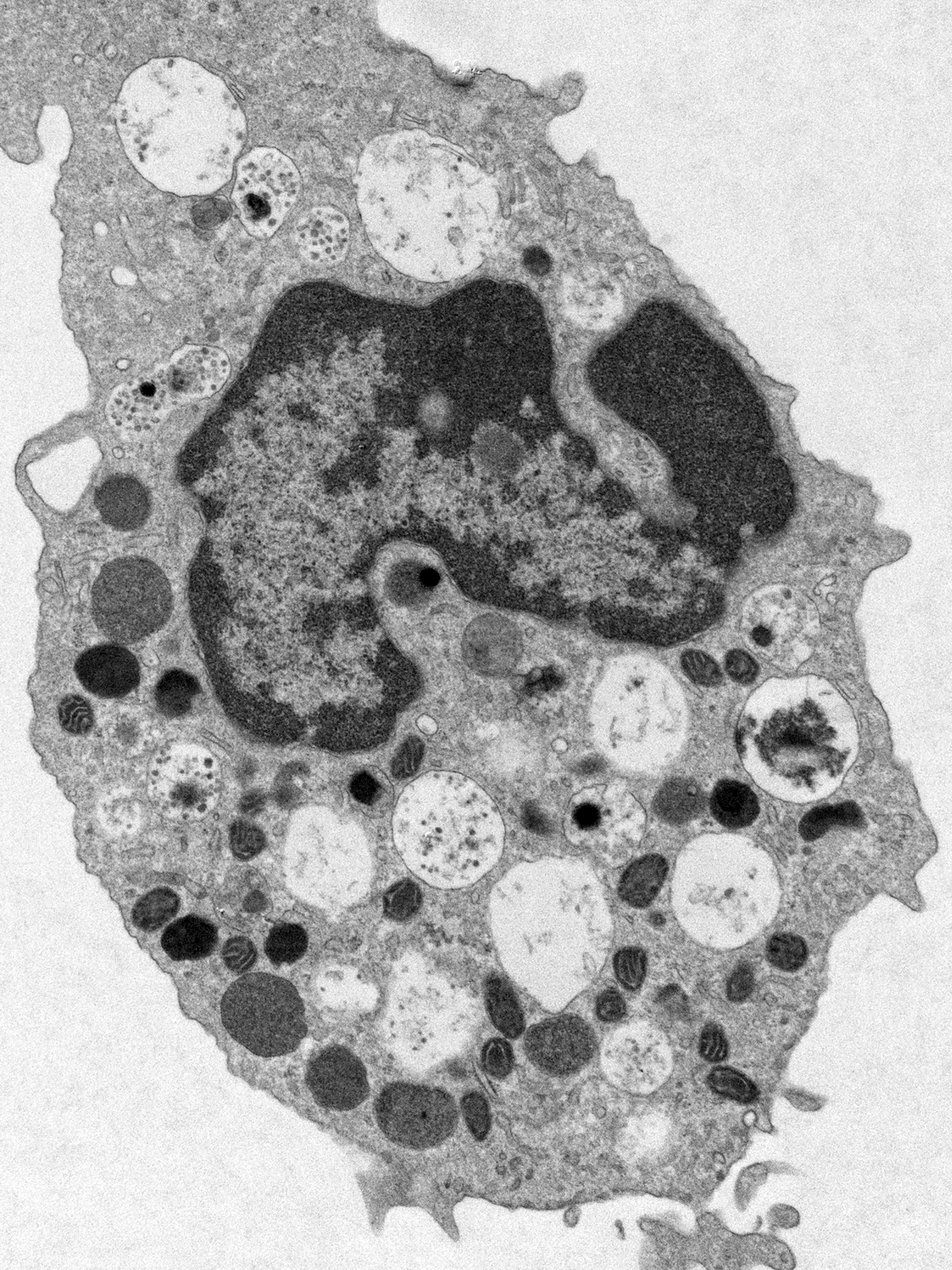
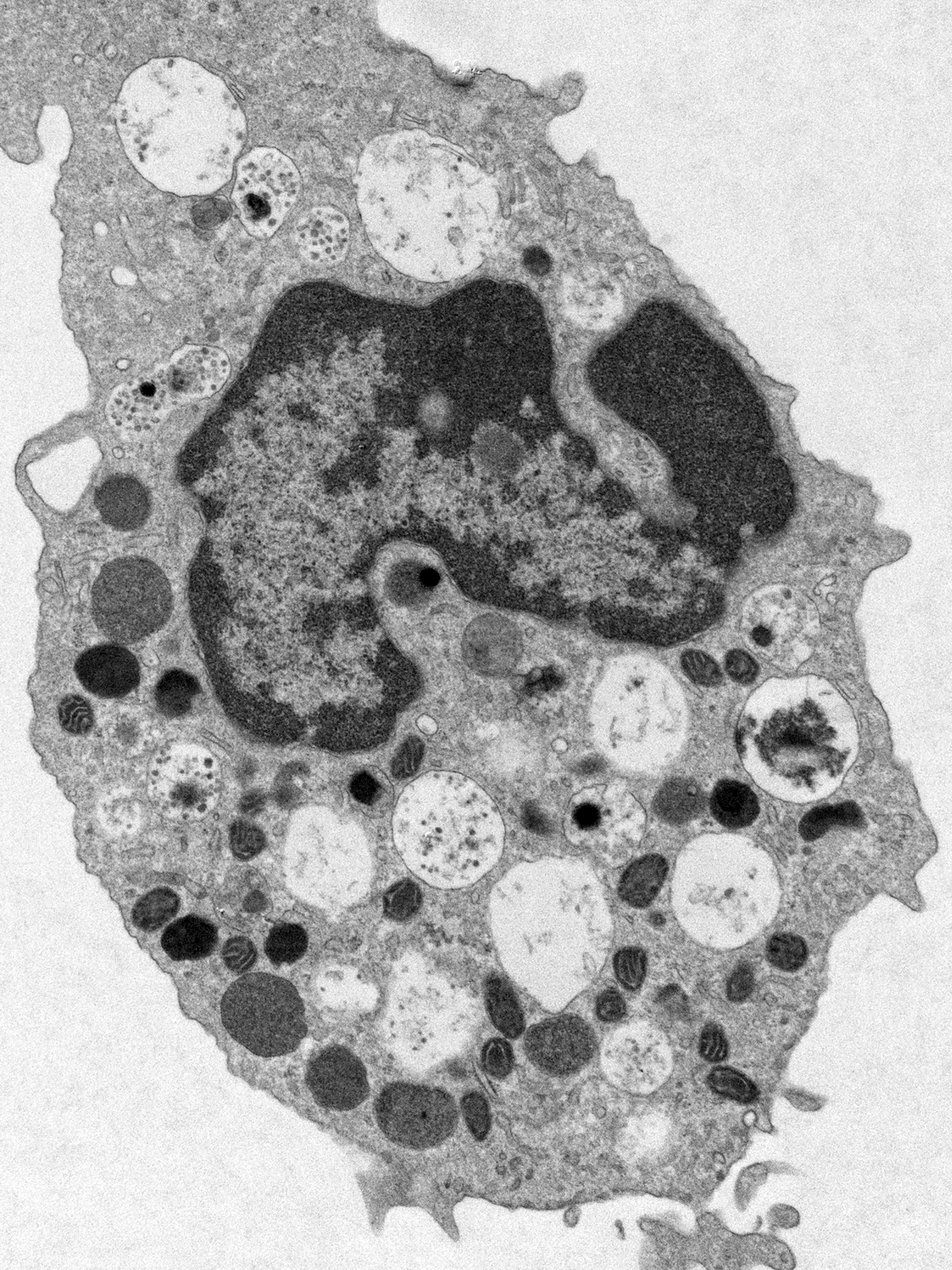
Allergic asthma is a complex condition characterized by pulmonary inflammation, increased mucus production, and epithelial remodeling, pulmonary inflammation, and increased mucus production—factors that contribute to airway constriction and breathing difficulties. Interestingly, individuals with asthma experienced reduced morbidity and mortality compared to the general population during the 2009 H1N1 influenza (swine flu) pandemic. Using murine models of allergic asthma which exhibit pulmonary eosinophilia, our lab demonstrated that eosinophils engage in crosstalk with CD8⁺ T cells leading to, decreasing reduced viral load and influenza pathophysiology. The Samarasinghe Lab investigates the underlying mechanisms of this response, focusing on the transcriptional regulation, immune cell interactions, and differentiation of eosinophil populations during respiratory viral infections.
 Characterizing antibacterial immune responses in allergic asthma during primary and opportunistic respiratory bacterial infections
Characterizing antibacterial immune responses in allergic asthma during primary and opportunistic respiratory bacterial infections
Eosinophils are traditionally recognized for their protective role against helminth infections, but they also possess antibacterial capabilities. Using a murine model of allergic asthma marked by eosinophilia, the Samarasinghe Lab discovered that mice with allergic inflammation exhibited reduced mortality, lower Streptococcus pneumoniae bacterial loads, and decreased lung damage and inflammation following co-infection with influenza A virus and S. pneumoniae. The lab is working to uncover the mechanisms by which eosinophils detect and eliminate opportunistic bacterial pathogens in the respiratory tract.
 Exploring the Role of Lung Microbiota in Asthma and Pulmonary Infections
Exploring the Role of Lung Microbiota in Asthma and Pulmonary Infections
Communities of bacteria residing in the lungs interact with immune cells and may influence disease pathogenesis. An imbalance between symbiotic and pathogenic bacteria in the lung can disrupt immune development and trigger inappropriate inflammatory responses. However, it remains unclear whether this dysbiosis is a cause or consequence of disease. The Samarasinghe Lab has shown that antibiotic treatment alters lung microbiota in a murine model of allergic asthma, diminishing the protective effects of asthma during co-infection with influenza A virus and Streptococcus pneumoniae. Ongoing work in the lab aims to uncover how crosstalk between resident microbiota and eosinophils contributes to protection against asthma and pulmonary infections.